Percutaneous Transluminal Coronary Angioplasty (PTCA) is a minimally invasive procedure that aims to open up blocked or narrowed coronary arteries, improving blood flow to the heart. As a common treatment for coronary artery disease, PTCA plays a crucial role in managing heart conditions and preventing serious complications such as heart attacks. This blog will provide an in-depth understanding of PTCA, including its procedure, differences with PCI, potential complications, and post-procedure care.
1. What is PTCA?
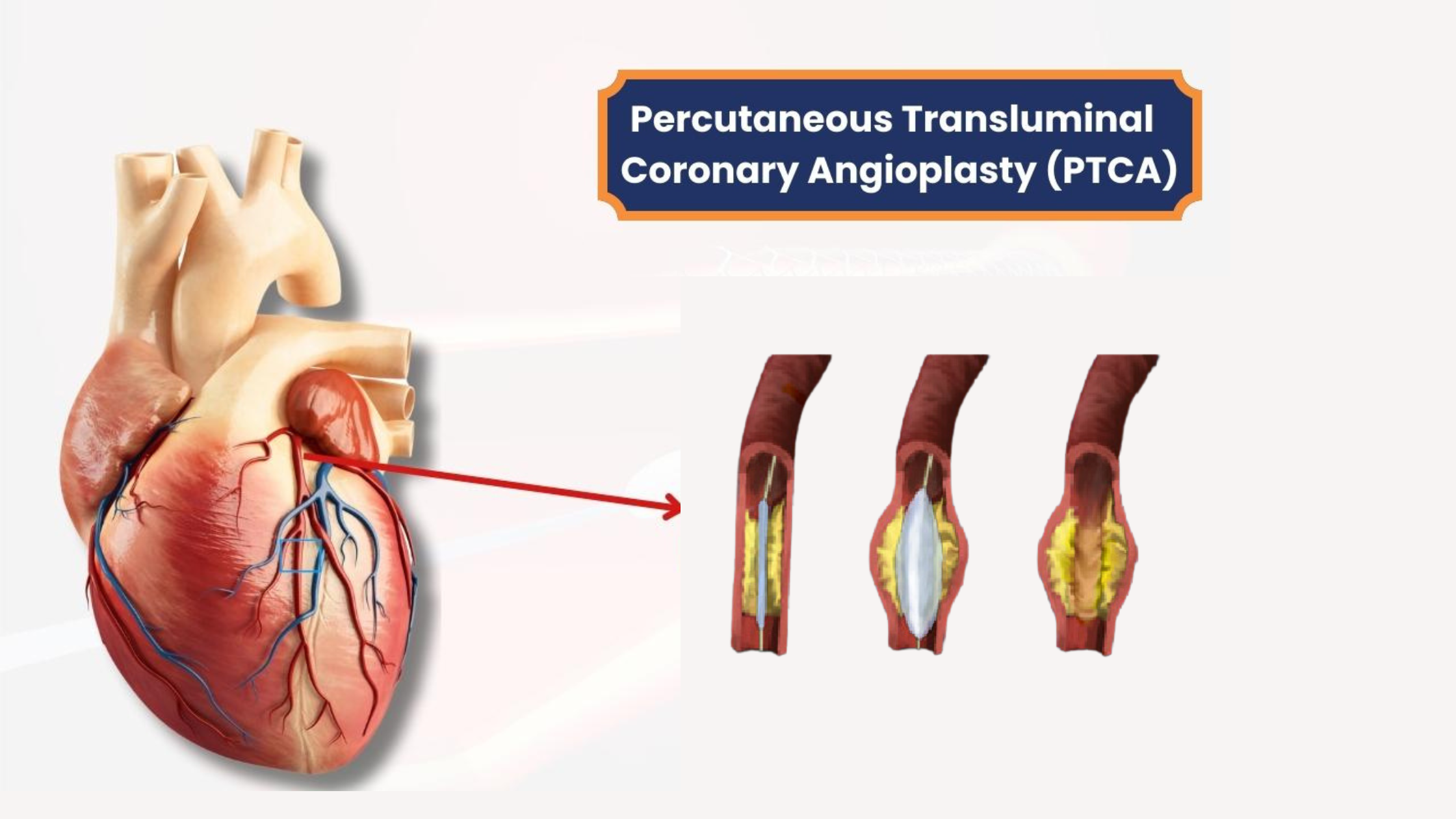
Percutaneous Transluminal Coronary Angioplasty (PTCA) is a medical procedure used to treat narrowed or blocked coronary arteries. These arteries supply blood to the heart muscle, and when they become narrowed due to plaque buildup, it can lead to chest pain (angina) or even a heart attack. PTCA involves the insertion of a catheter with a small balloon at its tip into the narrowed artery. The balloon is then inflated to compress the plaque against the artery wall, which widens the artery and restores normal blood flow.
2. PTCA Procedure: Pre-op & Post-op
Pre-operative Preparation Before undergoing PTCA, patients typically undergo a series of tests, including an electrocardiogram (ECG), echocardiogram (Echo), blood tests, and coronary angiography, to assess the extent of arterial blockage. Patients are advised to avoid eating or drinking anything for several hours before the procedure. Medications may be prescribed to relax the patient and reduce the risk of blood clots.
The PTCA Procedure
- Step 1: Catheter Insertion
A catheter is inserted into a blood vessel, usually in the groin or wrist, and guided to the coronary artery under X-ray imaging. - Step 2: Balloon Inflation
Once the catheter reaches the narrowed area, the balloon at its tip is inflated. This inflation compresses the plaque against the artery walls, widening the artery and improving blood flow. In some cases, the use of a drug-eluting balloon may be considered, which can help prevent the artery from narrowing again. - Step 3: Stent Placement (Optional)
In some cases, a stent (a small wire mesh tube) may be placed in the artery to keep it open. This is more common in PCI (Percutaneous Coronary Intervention) procedures. - Step 4: Catheter Removal
After the artery has been widened and, if necessary, a stent placed, the balloon is deflated, and the catheter is removed.
Post-operative Care After the procedure, patients are monitored in a recovery area. They may need to lie flat for several hours to prevent bleeding from the catheter insertion site. Medications to prevent blood clots and manage pain may be prescribed. Most patients can return home the next day, although they are advised to avoid strenuous activities for a few days.
3. PTCA vs PCI
PTCA and PCI are terms often used interchangeably, but there are subtle differences between the two.
- PTCA refers specifically to the balloon angioplasty procedure used to open narrowed coronary arteries.
- PCI (Percutaneous Coronary Intervention) is a broader term that includes PTCA but also encompasses additional procedures, such as stent placement and the use of other devices to treat coronary artery disease.
In essence, while all PTCAs are a form of PCI, not all PCIs are limited to just balloon angioplasty.
4. What is Percutaneous Transluminal Angioplasty?
Percutaneous Transluminal Angioplasty (PTA) is a procedure similar to PTCA, but it is used to treat blockages in other arteries outside of the heart, such as those in the legs, kidneys, or neck. Like PTCA, PTA involves the use of a catheter with a balloon at its tip to open up narrowed or blocked arteries, improving blood flow to the affected area.
5. PTCA Complications
While PTCA is generally safe, as with any medical procedure, it carries some risks. Potential complications include:
- Bleeding: At the catheter insertion site or internally.
- Blood Vessel Damage: Injury to the blood vessel where the catheter was inserted.
- Re-narrowing of the Artery (Restenosis): In some cases, the artery may become narrowed again after the procedure.
- Heart Attack: Though rare, it is possible for a heart attack to occur during or after PTCA.
- Stroke: A stroke can occur if a blood clot travels to the brain during the procedure.
- Kidney Damage: The contrast dye used during PTCA can cause kidney damage, particularly in patients with pre-existing kidney conditions.
6. Post-PTCA Care
After PTCA, proper care is essential to ensure recovery and reduce the risk of complications. Key aspects of post-PTCA care include:
- Medication: Patients are usually prescribed antiplatelet medications to prevent blood clots and may need to take them for several months or longer.
- Lifestyle Changes: A heart-healthy lifestyle is crucial. This includes eating a balanced diet, exercising regularly, avoiding smoking, and managing stress.
- Follow-Up Appointments: Regular follow-ups with a cardiologist are necessary to monitor heart health and assess the success of the procedure.
- Monitoring for Symptoms: Patients should be vigilant for symptoms such as chest pain, shortness of breath, or swelling at the catheter insertion site, and seek medical attention if these occur.
Frequently Asked Questions (FAQ) About PTCA
Q1: How long does a PTCA procedure take?
A1: The PTCA procedure typically takes about 30 minutes to 2 hours, depending on the complexity of the blockage and whether additional procedures like stent placement are needed.
Q2: Is PTCA painful?
A2: Patients are usually awake during the procedure but are given local anesthesia to numb the catheter insertion site. You may feel some pressure or discomfort during balloon inflation, but severe pain is uncommon.
Q3: How soon can I return to normal activities after PTCA?
A3: Most patients can resume light activities within a few days. However, strenuous activities and heavy lifting should be avoided for at least a week or as advised by your doctor.
Q4: Can PTCA be repeated if the artery becomes blocked again?
A4: Yes, PTCA can be repeated if necessary. However, the decision to repeat the procedure depends on various factors, including the location and severity of the blockage and the patient’s overall health.
Q5: What are the alternatives to PTCA?
A5: Alternatives to PTCA include coronary artery bypass grafting (CABG) surgery, medical management with medications, or lifestyle changes to manage coronary artery disease. The choice of treatment depends on the specific condition and patient preferences.
Q6: Does PTCA cure coronary artery disease?
A6: PTCA can significantly improve blood flow and relieve symptoms, but it does not cure the underlying disease. Patients need to continue managing their heart health through medications, lifestyle changes, and regular medical follow-ups.